Ep040: Sleep Study? What to Expect?--with Dr. Khosla
Seema Khosla, MD
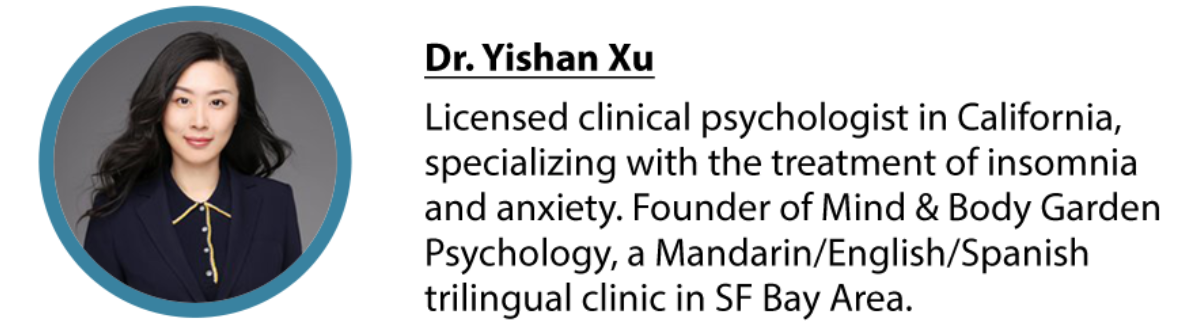
with Dr. Yishan Xu
TODAY’S GUEST
Seema Khosla, MD, is board certified in internal medicine, pulmonary disease, critical care medicine, and sleep medicine. She works in Fargo, North Dakota, where she is the medical director of the North Dakota Center for Sleep.
Dr. Khosla previously served on the AASM Task Force on Sleep Telemedicine, which developed a position paper for the use of telemedicine for the diagnosis and treatment of sleep disorders, and she was co-chair of the AASM Sleep Medicine Trends course. She is currently the chair of the AASM Consumer and Clinical Technology Committee, which developed a position statement on the use of consumer sleep technology in clinical practice.
WHAT WILL WE LEARN
RESOURCES
AASM’s new podcast can be listened here
https://aasm.org/professional-development/talking-sleep-podcast/
Dr. Khosla’s practice:
https://www.doximity.com/pub/seema-khosla-md
Our podcast interviewed the same guest: Dr. Chris Winter (see our episode 013)
https://www.deepintosleep.co/episode/013
Thank You for Listening!
Newsletter and Download Free Sleep Guidence E-Book:
CBT-I Courses:
Podcast Links:
Apple Podcast: https://podcasts.apple.com/us/podcast/deep-into-sleep/id1475295840
Google Podcast: https://podcasts.google.com/search/deepintosleep
Spotify: https://open.spotify.com/show/2Vxyyj9Cswuk91OYztzcMS
iHeartRadio: https://www.iheart.com/podcast/269-deep-into-sleep-47827108/
Support our Podcast: https://www.buymeacoffee.com/dryishan
Leave us a Rating: https://podcasts.apple.com/us/podcast/deep-into-sleep/id1475295840
Transcript
- 0:00
From my own clinical work, I find quite interesting that when someone come to me for treatment of insomnia or other mood disorders, I often check their sleep quality, how they sleep. And sometimes they will mention themselves have some kind of sleep symptoms that out of the scoop of insomnia, or they will tell me that either their spouse, or their parents actually snore heavily, quite loudly for years. And I often tell them well, other than our treatment to you for whatever your major complaint is, we have to consider based on the symptoms you just report to me, I think we need to consider either for you, your spouse, or your parents to have a sleep study then which is a test In a sleep center, and they often asked me what is a sleep study? What is sleep testing? So today, we have Dr. Khosla to really share with us what it's like to have a sleep test, a sleep study done, and during Kobe read what many sleep centers, especially their sleep center have done to really protect their staff and patient safety. Dr. Khosla also share different types of sleep disorders, and how sleep study can really help with the process of diagnose. Also, what are some appropriate treatment for certain sleep disorders once you get the diagnosis through a sleep study, for example, sleep apnea and in their center, how she follow up with patients through telehealth and to Really monitor follow up to keep good patient care. So if you or your family are struggling with sleep disorder or are waiting to get sleep study, Dan, but because co aid, you are encountering some difficulties. Hopefully this episode can give you some ideas, what it may look like right now and to help you reduce your anxieties about visiting a sleep center under Kobe. Welcome to deep into sleep. I'm your host Asian. Let's welcome Dr. Khosla. Okay. Welcome, Dr. Khosla.
- 2:40
Thank you for having me. I appreciate it.
- 2:43
So I'm really happy to have you here.
- 2:46
I have a quite a lot of questions for you. So I know you're the medical director at North Dakota center for sleep. And so I'm curious what, what you do they are what's your special Tea locally in the sleep center.
- 3:03
Sure. So I am a pulmonologist. My I did a fellowship in pulmonary critical care and sleep. But now I do 100% Sleep Medicine. So I see clinic patients and we do sleep testing both at home and in the lab and we take care of any any sleep disorder, not just sleep apnea. We take care of insomnia and restless leg syndrome and narcolepsy and at Pathak hypersomnia. So we we take care of any sleep concern that somebody may have
- 3:35
all this great. So sounds like a very wide school, you can see a lot of sleep disorders there.
- 3:42
Well, and you know, what I've always found really interesting is that, you know, I think sleep is a great equalizer, no matter who we are, whether we are educated or not, or wealthy or not, you know, we all need sleep. And so it's something that you know, we were Can't afford to ignore. And so many of us have undiagnosed sleep disorders, or we have this attitude of Well, that's as good as it's gonna get. And I need to accept that.
- 4:12
Yes, exactly. And also, as a psychologist, myself, I find sleep topic is such a good weigh in for other mental challenges and people love to talk about sleep and are okay with sleep, there are less stigma attached to that. And then when we start talking about sleep and treating sleep, and many other things can slowly happen.
- 4:35
What a great, you're right, what a great viewpoint. You're exactly right. You know, and why is that? We do have this mental health stigma, and I think you're right, there's such overlap between our mental health and our sleep. So I'm really glad that you can use that to open open the door and engage your patient that way. Do you find that they it makes them more willing to share with you
- 5:00
Yeah, more willing for me, I think it's make them more willing to share with me and the start realizing, oh, seeing a therapist seeing a psychologist, and it's not as scary. And actually all my sleep symptoms, especially insomnia for me to treat, my insomnia can get better. And then in the process, I realized, Oh, actually, I'm anxious, or actually, I feel sad, often, there may be some other things. So I think they it's just a higher level of acceptance, to be willing to face whatever is a deep challenge they have.
- 5:36
Well, isn't that interesting? You know, my I joke about this a lot. But in our sleep clinic, we go through a lot of Kleenex, and my friends make fun of me. What do you make your patients cry? And I said, Well, you know, it's not I think so much of like you talked about with insomnia is for some reason, I think we have been programmed to believe That if you have insomnia, you need a prescription for a pill. And that's it. And really, I think we kind of owe it to our patients to try to figure it out a little bit more. And so I don't know what you know, you know, you kind of hear a lot of childhood sexual trauma, and you hear a lot of marital issues, and you hear a lot of the other things that are contributing to insomnia. And then when people have this, I mean, I suppose it's kind of like a safe space to talk about it. You can see that they start connecting the dots, and they realize that, Oh, this is why I'm not sleeping. And yeah, I see why you think I need to go see a therapist. I found it interesting that you said that people are somewhat reluctant to see you. And I wonder if we should, that's something that we probably share that a lot of people that are in sleep clinic are there because their wives or husbands have sent them and they really don't want to be there and they really don't Have a sleep test and you really don't want to work out. But then if you can pull that out like you do with your patients, and you show them how the thing that really bothers them might be linked to something that they are a little bit uncomfortable talking about. And then you lead them, and you connect them to that. And I think that's very impactful.
- 7:24
Yeah, I totally agree. I think we definitely share some of this experience, and we can see how good people are at avoiding things. Yeah, and I also know a lot of different sleep disorders other than insomnia like narcolepsy, it can really harm or impact our quality of life.
- 7:48
Isn't it amazing? narcolepsy is such a tough one. You know, I think people you know, for lay people. I think a lot of people think it's funny, right? It's comical, like the guy on TV. who falls asleep in a soup? And people think it's really funny. And they don't realize how debilitating this can be. And it's more than just falling asleep, right? There's so much more to it. I mean, think about how that impacts you day to day when you've had a night or two of not sleeping well, and you're exhausted and you can't think the next day. Right? Imagine if that's your every day. Yeah. And then trying to articulate that to your family and your friends and people who don't understand and who, who think that you're lazy, or that you just why don't you just go to bed earlier and you're just spending too much time on your phone and they and they don't get it. And I think that is one of the hardest things, I think for our patients is that if you have a diagnosis like cancer, for example, everybody understands that and everybody kind of gets that it's not your fault. And this is a horrible thing that happened to you. And when you Deal with something like a sleep disorder. I think there's not that same understanding. I mean, I'm not equating the two by any stretch. But there is still that idea of people have sleep disorders that profoundly impacts their day to day. And yet, so many people assume that they're lazy, or they're doing it to themselves, or they're just staying up too late. And that's why they're sleepy without recognizing that there may be a true underlying sleep disorder that no matter how much they sleep, they still don't feel rested.
- 9:33
Right, exactly. I think that's such a important point for a lot people to know that this layer of stress this pressure did not only add to themselves, they're confused what's going on with me? Is there something wrong with me? Am I just lazy and there's so many like external stress from from people around them. I know people who are diagnosed with sleep disorders and lost their lovers, their partners and people around them just don't understand think they are weird. And some of them have to quit their their job and cannot finish their school. It's quite challenging. It could be really severe.
- 10:17
It really can. And sometimes even I remember this nurse, years and years and years ago, she always worked nights. And I knew her from my pulmonary days and critical care days. And she had narcolepsy. And it was one of those things that it It took her a long time to get a diagnosis. And she managed it very well. And she just chose to be a night shift worker because that worked better for her. And she was very successful at it. And so I think with the right support in the right treatment, yes, you know, people can have these very full functional lives, but that social support is so important. So her husband was Very, very, very supportive of her. And I think that made a huge difference for her and her in her outcome.
- 11:06
Yeah, yeah, definitely if people we love people wronged us really understand or try to understand and try to learn how to support us how to support patients who are struggling with some kind of sleep disorders that can definitely even psychologically, I think that make a huge difference for sure.
- 11:28
Yeah, and I think the same even goes with C pap. So spouses who accept the C Pap, I think, you know, and they're very encouraging. So one of the complaints we get in clinic all the time is, you know, see pap just isn't sexy. I don't want to where this comes up all the time. And you know, and you try to you try to switch it, you know, you try to say well, but it's a lot sexier than like the gasping and choking and, and if this person really cares for you, right? It's not Going to, you know, it's not going to be that big a deal. And I know you know that if you look at somebody that you care about, you feel better knowing that they're on a CD Pap, right? And so it's just one of those. I had one. I had one lady years ago now, she had gone through divorce, and she was dating, and she came into clinic and she's like, so listen, my boyfriend is going to spend the night for the first time. She said, What do you think I should do with my C pap? And I said, Well, you know, I want you to wear your C pap every time you sleep, right? So I want you to wear but ultimately you have to decide what you want to do. And so she really thought about it and she put her seat away. And her boyfriend came over to spend the night and the first thing that he did was unpack his seat, Pap, and then she looked
- 12:51
great, and so she unpacked her seat.
- 12:55
They will actually they wound up getting married. It was such a lovely story. Wow, that's so sweet.
- 13:02
A great example.
- 13:04
So yes, they were both very supportive of each other. So I thought that was really kind of cute. She was very excited to tell me about that next time we met.
- 13:12
Yeah, yeah. So that's a path. I know it's type of treatment. And you mentioned sometimes it takes a very long time for people to get diagnosed, gets the right treatment. And some guest I interviewed on my podcast before, they had similar problems took their took them like years, like some of them, around 10 years are more than 10 years to guide to get a diagnosis. And so I know one common way to be diagnosed with sleep apnea, for example, it's sleep testing, and to be in the lab or there are other ways, right? What's the barrier for people to get diagnose?
- 13:55
You know, I think so much of it depends on whether it's on your radar. Or not. So if what we've seen is that especially as women, women can be under diagnosed, because we don't necessarily have the same symptoms as men, you know, the guys all like they read the book, right? So they gasp and choke and turn blue and their bed partner says honey you need to go in. Whereas for women, we sometimes are a little bit more subtle. And we have more apnea, maybe in you know, later in the night, when our bed partners are asleep. And maybe we have insomnia rather than hyper somnolence. And so a lot of the time as women, we get treated for the hypertension and the depression, rather than the sleep apnea, that might explain all of it. And so I think that has been you know, you have to be able to think of it before you can diagnose it. The other limitation I think has been testing. So you're right We've always had this in lab test, which is a great test, but it is, you know, it's a lot of wires and you have to come in and be away from your family. And there's costs associated with it. There's a home sleep apnea test that which is kind of nice that you can do it at home. So if you ask the question, is a home sleep apnea test as good as an in lab study? The answer is no.
- 15:25
But
- 15:26
if you ask the question, is home sleep apnea testing good enough? for regular obstructive sleep apnea? The answer is yes. With a with an Asterix, right. So if we, if we catch it at home, great, but most of the tests that we use at home, don't, they can't tell if you're awake or asleep. And so then you won't have sleep apnea, if you are awake, and so then the numbers get watered down. And so one of the things that we've been trying to do You know, forever, we have really been trying to show people that sleep is really, really important. Right? And, and there's been this cultural shift, I think, where we used to be very proud of staying up all night, right, it was his badge of honor. And now people are really making it. this cool thing that hey, this is my mask, and I'm gonna go to bed now. And this is my bedroom and look how great it is for sleep. They're really making that more important, which I love. We've made a very glamorous now to just go to sleep. And so part of that, I think, is that we have this heightened awareness of the importance of sleep, and I think we owe it to our patients to make it easier to get tested. So a lot of testing is in the home now. One thing that we have been trying to do is make it even more accessible. You know, one of the bottlenecks is, well, you have to go to your doctor and have to get a referral. And you have to do this. And you have to do that. So hey, you know, people get tired, right? They don't want to make 10 trips to do one thing. And so we're trying to figure out how we can improve sleep health. And so we know from various studies that 80% of sleep apnea is undiagnosed. I mean, that's huge.
- 17:29
That's a very high number.
- 17:30
It's very high. And, and I think a lot of the time, people are like, yeah, I probably have sleep apnea. But I don't want to receive pap and I don't really care. And so I think it's a matter of showing them that, well, sleep apnea actually is an important thing. It's more than just snoring. Right? And these are the things that can happen to you and how can we make it easier for you? You know, treatment doesn't have to be a C Pap, right. There's lots of ways we can treat sleep apnea. Let's find something that works for you. Let's try to figure it out. So if you look at and this is something that we're, you know, everyone's talking about, but there hasn't been really good data yet. But if you look at the patients in New York with COVID, the top three populations of people who didn't do well, diabetes, hypertension and obesity, that's kind of the trifecta of obstructive sleep apnea. And if you if you factor in 80% of those are probably undiagnosed, right? Is sleep apnea playing a role and why people aren't doing well. I mean, we know sleeps important for our immune system. We know that sleep apnea has this inflammatory component. Right. So right is this part of it? So then, of course, we bring it back to our family members, right? And so my mom's on a C Pap, and I'm very, very careful to make sure that she stays healthy. And you know, my brother delivers groceries here. My mom and my brother both live in Canada, where I'm where I'm from. And in my mom's a family practice, doctor, and I've been teaching her how to do telemedicine because I don't really want her to go physically see patients. And make sure you clean your sleep app. Mom, make sure you wash your hands before you touch your sleep app, like all of these things, right? Right. So we're trying to do that to our patients to, you know, with COVID, we've had to shut down the lab. And, and so this has been really hard, because we know that sleep apnea is really, really important to diagnose and treat. But we also want to keep patients and our staff safe. So it's kind of funny, we've done a crazy amount of things to try to do that. And if I showed you all of the documentation and all of the plans that we've had, you would you would laugh, because it's it's really, we've got so many different versions because things change all the time. Right. So I'll send out an update, you know, to my colleagues, and I started As soon as I hit send, some other article will pop up. So, now we we have so I wear different hats in my life. So I've got my my clinic hat in Fargo. But then I'm also a medical advisor for a larger company called med bridge healthcare. And they do sleep testing across the country. And so then we're having to look at, you know, the lab in New York, for example. And in North Carolina, and in the Dakotas, and in Minnesota, in an Iowa like what, you know, what can we do differently? And how do we figure this out overall as a company, to keep everybody safe when there's so much variability, you know, in the region, so we kind of always go back to, okay, what I put my mom in the lab, right as a patient or as a tech, and so we have PP for our techs. We screen our patients twice. We screen our staff
- 21:02
We, we took our labs used to be really, really pretty, really pretty. They look like hotel rooms just beautiful. We took all of that sort of pretty stuff out, like all the little like the clocks and the, you know, the little decorative things. We took it all out because we didn't want that to be a source of infection. And then we're really picky about who gets into the lab. And we look we, we have this ability. There's a website that lets you look at Coronavirus per county and then you can look to see whether it's going up or going down and whether it's fast or slow or whatever. And so then we kind of make a plan for that lab in that county according to what's happening. And then we have these boxes that we invested in these UV boxes and so that our Tech's can disinfect their phones and their keys, you know, whatever. And the rooms are all swept out and the we have mattress covers that are waiting And pillowcases that are wipeable and all of these things, and we have viral filters in there. And we have closed circuits. I mean, it's unbelievable. These things that we're we're trying to come up with just to keep people safe. And and also we're just not, you know, we're converting as many people to home testing as we can. We're using disposable equipment. I mean, this whole thing is really up ended our, our sleep world. And so we still feel this obligation, right? Like you still have to take care of your patients, and you still have to protect your staff. And if we're going to be dealing with this for 18 months, we better figure out how to do it well.
- 22:42
Yeah, that's amazing. A lot of detailed really details you all have to manage and pay attention to especially Williams, like nationwide, different locations. That's a lot of work, but the same time, I think as potential patients when they hearing all the steps when they can see all this changes, they do feel safer.
- 23:07
I hope so. Because you know, that's our goal that so so at first, the easy thing to do is just say, Oh, we got to shut everything down. And I was talking to a friend of mine. And he he made me look at it differently. So he had a patient who was young ish, right sort of mid 40s, I think or something who was supposed to come in for a sleep study. And because of COVID, he didn't get to come in, he didn't get to come in. He didn't get to come in. He got delayed, delayed delayed. And when he finally came, his oxygen levels so low, they sent him to the ICU. Oh, wow. And so he was upset, because, you know, he's saying you guys were not, you know, this is not right either. And I said, Well, you're right. It's not right. So we have to figure out who you know, we have to sort of do that a second. Have, it's really important for this guy to get in. Whereas this guy could probably wait. Right? Or maybe this guy, we can start on C pap without a test. But I don't know, right? We're doing all telemedicine for example, like we just shut down our clinic. And I see patients, you know, via telemedicine now. And so that's been changed. I mean, I've done telemedicine for 10 years, but I've never been able to do it in someone's home. We always did it from our clinic to someone else's clinic. Right. And so this is, it's familiar, but it's still different when you have to have it in patients homes. So that's been interesting. You know, and I think Above all, we all just, you know, you have to do what's right for your patients. Like that's all it that's what it comes down to, you just have to do right by your patient. Yeah, and because sleep apnea or different sleep disorders can still be very severe and can lead to, like really bad house consequences. So that's another issue. level of safety? No, you're exactly right. And, you know, I mean, you don't want sleep apnea. You're right. It does cause, you know, stroke and high blood pressure and diabetes and memory problems and all of that. So it is really important to treat. So when you, you know, on paper when the CDC says, Okay, well, this is an essential service. And this is not an essential service. I mean, I get it, you know, getting your toenail removed, it's probably not super emergent, and having your heart attack that's emergent. That's really, really clear. But I think what's less clear is a sort of middle ground that, okay, today, your sleep apnea is probably not going to kill you. But if we wait two years, probably that's not great either. And so there has to be middle ground and how can we do this safely? for everybody involved? I think that's a huge concern. And definitely not sleep only What about your practice? Are you seeing telemedicine patients?
- 26:03
Yeah, so my practice is all like, we are therapists. So we have switched mostly outside to tele house. But for high risk patients like for patients have. So as suicidal ideation or even intentions or some kind of plans, we think they're in danger. We are trying to still see them face to face with masks on with a towel may or may. therapists have to we have to have certain regulations to make sure everyone's safe. So we are trying to wipe the whole office every day all that so definitely, I think it's a it's a adjustment for all of us across different settings.
- 26:52
Isn't it funny to that how your office changes so even the week before we finally shut down our clinic we did didn't let anybody sit in the waiting room, we'd make them wait in the car. And we didn't let like, other people come to the appointment. It was just, and we in my clinic is small. And it's hard to get six feet between my chair and the patient where the patient sits. But we did try to move everything as far as we can, without it being so obvious, like shouting across the room at somebody. But, but it's a things I think that you, you know, we've done forever. You know, I've been there for 11 years, you know, and you get used to the way things are and then I think it is important to look at and say, Okay, well hang on, why do we need this? Like, we got rid of all our magazines, in the waiting room? You know, I'm like, Oh, yeah, we probably don't need those. That's probably a good thing. We don't have candy dish anymore. You know, we just have coffee for our patients and, and that sort of thing. So we've kind of gotten rid of all of that.
- 27:59
Yeah. Yeah, it is very interesting. I hear stories from my colleagues, they are actually changing their office they totally switching offices because their old office is too small to keep six feet. So they're actually moving like you know, try to rent a new office can be a little bit larger. And for me myself, I try to have a couples therapy with, you know, multiple people in the session together. So all of us like at least three of us, sometimes family therapy has more people. We all have to wear facial masks, talk to each other. Keep a certain distance be very cautious, no handshaking anymore for one to two hours. Sometimes a session goes really long. It's very, very uncomfortable.
- 28:48
So I bet that is hard then because people people read your facial cues.
- 28:53
Right?
- 28:55
So is his Do you have you found that that's been a challenge wearing a mask?
- 28:59
Definitely. It's harder for me to read their facial cues to, especially as a as a provider for therapy. I want to know what was going on and they're weird. There are subtle dynamic between couples within a family. So I would say definitely, it brings more challenges. And I'm still trying to get used to how to just get enough information from their eyes, from their body gestures
- 29:32
in session. It's hard though, you know, that was one thing that I was what I'm imagining, you know, because some of our patients have not wanted to do telemedicine and so we're trying to figure out well, when will we open the office again, and I'll you know, we'll probably still do telemedicine and then have an in person, maybe at like, nine you know, and then due to tellement patients And then have another person come at like 11 so that we're separating them. But then I also was thinking about, well, you know, part of what I do when I evaluate them as I look at their, you know, I have them open up their mouth and I look at the back of their throat. So, for me, I've actually been able to get that really well from not always pretty well, with telemedicine. And so, and it's funny in some respects, because I'm trying to guide people to show me the back of their throat through their camera phone. And so I've looked at I've looked at a lot of ceilings, I've looked up a lot of noses a lot. And so, that's been interesting. I have to, I haven't quite gotten it down for how to convey how to do this to patients. You know, and it depends on what they're if they're on a tablet or a laptop or on their phone. And then I have an apple and I don't have an Android and I'm not really sure where the camera is on an Android but I need to figure that out so that I can help people He should get a better view. And so that's been interesting. And so I feel like that is, in many ways safer than me, actually, you know, opening up their mouth and taking a look.
- 31:14
Yeah, for you sounds like totally. That's actually it could be risky if you have to be so close to them and really need to have a closer look to their throat. And if the camera angle is right, that could be so much more clear with nowadays the technology the cameras are actually are quite good.
- 31:35
I'm actually surprised at how good the Emmys some of them of course, it depends on their internet connection, and their phone and that sort of thing. But some I'm just kind of amazed. I've been taking these pictures even, you know, just to show I'll grab a screenshot sometimes. And then I will share my screen and show the patient what I'm looking at. And I'll show them like, this is that dangly thing in the background. Have your throat and it's really read. And this tells me that maybe a sleep apnea. And so then it's really interesting because I, I can't really do that when I'm in person looking at their airway, I can't really show them their own airway unless I have a mirror or I take a picture with my phone. But this way I can share the screenshot during our visit. And then I delete it. And then you know, it's been, it's been interesting. And then they can also see the picture that I can see. And I think it gives it more legitimacy. Almost, I don't know, we've been experimenting a lot, you know, every day is different. Yeah, sometimes my one platform won't work, it'll be really laggy and then I'll call it another one on my phone. And then I'll have to do this. And then every so often, I'll just have, I'll be like, I'm just going to call you and I'll just pick up my phone and call them. So it's been it's been really interesting and I've enjoyed seeing how patients that I've known forever have adapted to it. You know, and even new patients, it's been really interesting to see how, you know, we all do have to figure out how to do this. Right? Because yes, you have to figure out our new normal.
- 33:13
Right, exactly. I totally feel the same and some, some patients actually quite enjoy it and myself kind of enjoyed the exploration with them together and figure out technical issues together and try to because now it's telemedicine sometime, we can definitely do more like I see children also with children. Sometimes they're so excited to share their screen with me to share some games they're playing some YouTube videos with me which is not happening in the in the office. Oh my gosh, how
- 33:51
adorable is that though? So they're more engaged.
- 33:55
Yeah, in ways many of them would love to show me their room where means a lot for children want to share to a provider that their little secret their their, you know toys, the law they want to share, they would love to talk. So some parents are surprised because some parents told me their children actually never Skype or video talk with any family member for more than 15 minutes before but they could stay in session for a whole 45 or 50 minutes and don't want stop. Well, we're still deliver some intervention in a fun way. So it's interesting
- 34:36
isn't that I find that it's kind of made us challenge. You know why we do things but also I think it makes us a little bit more creative in terms of, you know, what we want to see. So I've kind of enjoyed that too. You know, I had a lady that showed me her legs and showed me how swollen they were and she you know, I kind of guided her to well push her finger and then let's see what it looks like. And she can show it to me and, and even just looking at the side of somebody's face, you can see if their jaw sits back a little bit, you're like, Oh, you know what, that's a risk factor for sleep apnea, or you talk about, like, you share your screen, and you review the data, or you review this new cool thing that came out. Or they have their fitness tracker, right. And then you can share it and you can ask to see their screen too. And so it's been, it's been this exploration. That's been really, you know, I mean, yes. frustrating. Sometimes, of course, you know, I have two kids that are distance learning. And so they both have, you know, Google Hangouts, and then I'm trying to do telemedicine. So, you know, we've upgraded our internet twice. And I called and she's like, you cannot possibly be having problems. She's like, you're on the most like hugest bandwidth we have.
- 35:56
Like, you can't possibly be having problems still. I'm like, I am
- 36:02
So it's just that part's been interesting. You know, I have, I have these two dogs. And so they will sometimes try to make a guest appearance. You know what I'm trying to get them out of the way without letting on that. Got this giant dog that's trying to get my lap. But I think most especially for patients that I've known, you know, I think it's, it's a little bit different because they already know you and they kind of, you know, you have that relationship with them. I did have a guy the other day that I first met him on a telemedicine visit in his home. I met his grandkid and his dog and we sent out a home test to him and and he had sleep apnea. And so yesterday I saw him full circle. So I saw him before he had been diagnosed and then I review the test with him. I reviewed his c pap information. You know, we answered questions, and he'd lost 10 pounds. Since he's been on feedback. He felt pretty good. You know, he had his complaints about the mask and things like that, which I totally get. But it was, it was kind of that was the first person that I had done that full circle with. And so I thought that was really kind of a milestone that we've been doing this long enough to have circled back around with our patients, you know, and to sort of check in with them to see how things are going. Yeah.
- 37:25
Wow. That's amazing to to be able to see them and be wisdom, this whole journey, mostly through telemedicine, right. Yeah.
- 37:33
Right. And for the first so yesterday, I, I had a lady and I've known her for years, but she was having trouble with her machine. It was giving her a headache. And she'd already stopped wearing it. And so we kind of talked about this, you know, because she's in a higher risk group for COVID. And we talked about, Well, you know what, let's let you know you've already stopped using it. Let's maybe check it And I've never been able to do this, but I can see her next week. Because a I have ruined my clinic now. And be it can be I don't have to feel guilty that I'm, you know, putting her in a car and asked her to drive. You know, she'd pick up the phone and, you know, like 15 minutes or 20 minutes and it's not a big deal. I can do it over lunch. I have never I can't remember in the last decade ever being able to bring somebody back next week. Like that just never happens. And so that's been really interesting. You don't have to see how she's doing next week. But that's been kind of cool.
- 38:37
Yeah, gave us a lot of flexibility and much better patient care in a way that they don't have to schedule time to really come in his phone call away. There's a way to, to figure that out.
- 38:51
Right. Amazing. But I have I do think that it has kind of uncovered these sort of those social determinants of health disparities. So I, I have a patient that we've been trying to get, and she doesn't have a smartphone, she doesn't have a computer, she doesn't have anything like that. So we're just doing a regular phone call for her. And so you can definitely see that people who have access to this technology are their advantage, right? And, and they get to play and they get to be part of this new paradigm. And the people who don't have access to it, it feels like almost like another door is being shot on them. Right, it's another thing they don't get to engage in, and it puts them further and further, sort of on the outside of what we're paying attention to. And that bothers me, you know, and I don't know I've been looking into their companies that will mail out like a tablet, and a third like a, an ear thermal thermometer and I can't remember something to look in your ear or nose or something I don't remember but they'll nail it to somebody and they'll have a little modify so that they can convert like cell signal into internet signal for the for that device. And I mean, it's interesting, right? Is that a way to do it? But then, you know, is that covered by insurance? Like how do you? How do you get over all those barriers? Right? And how do you still help your patients?